In 2016, a baby was born to three parents: two mothers and a father. Doctors used a new 3-person in vitro fertilization (IVF) procedure to deliver a boy carrying three sets of genetic material. This article will explore how and why we perform 3-person IVF, the medical and ethical issues surrounding it, and the limits of modifying DNA.
3-person IVF creates a baby using three sets of DNA. The father provides a complete set of genes through his sperm cells. However, the mother provides only her nucleus DNA, with a donor providing the mitochondrial DNA. This process prevents the birth mother from passing down defects in her mitochondria. 3-person IVF is controversial because we don’t know the long-term effects of genetic engineering.
Why Choose 3-Person IVF?
Deadly Mitochondrial Diseases
If you’re worried, a baby with three parents isn’t a mutant (not in the X-Men sense, anyway). It’s a form of gene therapy that helps parents conceive a healthy baby when the mother carries faulty mitochondria in her cells.
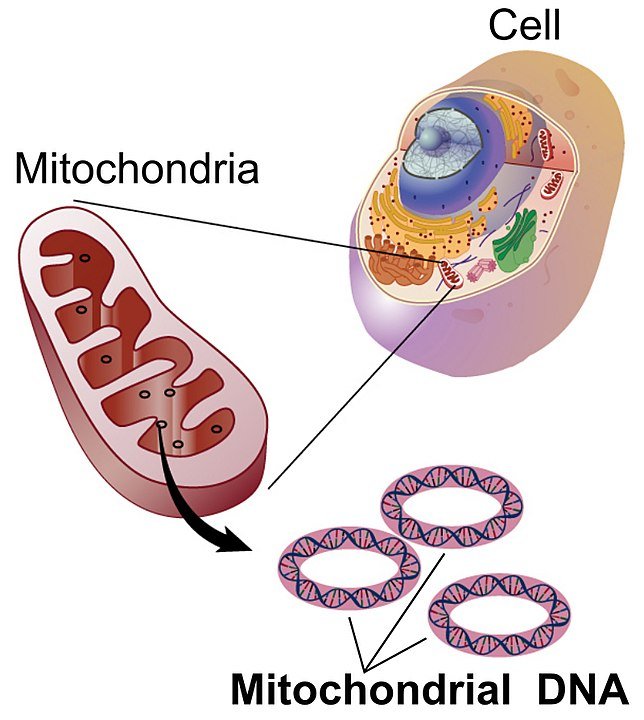
Mitochondria are cellular organs found in almost all of our cells, responsible for producing the energy we need to survive. They also carry their DNA separate from the rest, which is stored in the cell’s nucleus. When humans reproduce, the child only inherits the mother’s mitochondrial DNA.
However, this means that genetic defects in the mother’s mitochondria are also found in the child. Faulty mitochondria in children affects their growth and development, and in more serious cases, leads to severe neurological disorders and even death.
Mitochondrial diseases affect 1 in 8,000 live births, making them as prevalent as childhood cancer. A 2016 research study showed that 14% of children with mitochondrial diseases do not live past the age of six.
Having a Third Parent Prevents Genetic Defects
This is where 3-person IVF (in vitro fertilization) can help. The birth mother’s nucleus is extracted and inserted into a donor mother’s egg cell, creating a hybrid egg cell. This cell carries the birth mother’s DNA in the nucleus, with fully functional mitochondrial DNA from the donor.
The rest of the procedure proceeds like a typical IVF. The hybrid egg cell is fertilized by the father’s sperm cell and is implanted into the birth mother’s uterus, growing into a fetus that carries three sets of DNA!
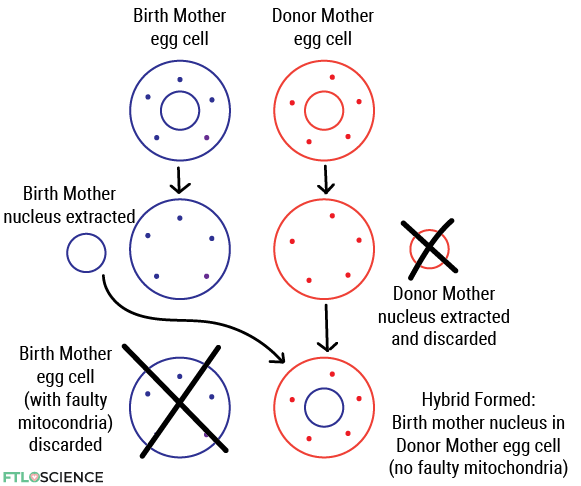
3-person IVF results in the child having three sets of genetic material, but only a tiny proportion of it comes from the donor mother. In context, the mother and the father contribute 20,000 genes to the child, while the donor mother only provides 37 mitochondrial genes.
The success rate for 3-person IVF is 20%—with only 1 in 5 embryos developing normally—compared to 50% in traditional IVF procedures.
The First 3-Person IVF Baby Using this Method
In April 2016, a boy was born in Mexico through the first successful transfer of the birth mother’s nucleus into the donor’s egg cell. His parents were a Jordanian couple who previously had two miscarriages and lost two children to Leigh syndrome. Children with this disorder do not usually live past the age of 3.
Leigh syndrome is caused by a genetic defect in the mother’s mitochondria, prompting the couple to seek genetic counseling to conceive a healthy child. Although there have been no public updates since, the doctors who worked on the procedure published a study in 2017, confirming the child’s good health at seven months old.
Concerns Surrounding the Procedure
3-Person IVF Isn’t 100% Safe and Effective
Extracting the nucleus from the birth mother and inserting it into the donor’s egg cell is a complex process. As a result, some of the birth mother’s faulty mitochondria may also be transferred to the embryo. This can result in the child developing less severe forms of mitochondrial disorders.
Similar 3-person IVF procedures have also failed in the past. In the 1990s, scientists injected donor mitochondria into an immature egg cell to treat infertility. However, signs of Turner syndrome (missing crucial genes in DNA) resulted in spontaneous miscarriage of the fetus. In another case, the procedure was successful in delivering a baby. However, the baby was diagnosed with autism at 18 months of age.
Furthermore, genetic engineering techniques are recent developments in science. We don’t fully understand the long-term effects of modifying DNA. Genes work in complex ways, often with multiple genes affecting a single observable trait. For example, editing a gene to cure a disease might cause another process to malfunction.
Legal Issues
Countries have strict regulations around gene editing techniques, as we don’t currently have a clear picture of its consequences. As it combines the genetic material of three parents, 3-person IVF is only legal in a handful of countries, including the U.K. and Australia.
In the United States, three-person IVF is illegal because it involves editing the DNA of sex cells (sperm and egg).
In the first successful birth of a 3-person IVF baby, the Jordanian parents and the U.S.-based team of doctors had to fly to Mexico to deliver the child since the procedure was banned in their home countries.
Ethical Concerns
Selecting specific traits that parents pass onto their offspring is another grey area. Some also argue that DNA editing techniques like 3-person IVF inevitably lead to future human enhancement. This is the same issue faced by designer babies—babies genetically engineered to be resistant to certain diseases.
In the future, will it be possible to edit or select certain facial features genetically? Can we alter our DNA to be stronger, faster and smarter? Where will we draw the line when it comes to genetic engineering?
The Future of 3-person IVF
A single successful case is all we have to gauge the technique’s viability, suggesting that more studies and trials are required. The flip side is that the only way to confirm its safety and effectiveness is by performing more 3-person IVF procedures, creating an ethical dilemma.
Being an expensive non-medical procedure, IVF also exposes a bias toward people who can afford it. Regular IVF costs US$15,000 per cycle, with three-person IVF likely to cost much more.
Another issue is the cost-benefit of researching techniques like these. Investing in research that aims to help children who suffer from genetic disorders might be better, benefiting families regardless of their income.
Although we now know that a baby can inherit the DNA of 2 moms, the procedure is unlikely to gain widespread appeal. 3-person IVF currently raises more questions than it answers, such as:
- Can one successful case prove its viability?
- Being an expensive (currently non-medical) procedure, is it right that only the rich benefit?
- Should our focus be on helping babies with genetic disorders lead normal lives instead?
- Will genetic engineering techniques change the future of our species?
About the Author

Marjory was a junior science writer at FTLOScience from October to November 2022.




