Have you ever wondered why we get fevers when we’re down with the flu? The immune system is a highly complex and efficient system of cells that carry out specific processes at a molecular level. Each one of these processes relies on another, working 24/7 to keep you feeling fine. This also means that when something goes wrong, the fragility of the entire system can be exposed. We explore the workings of our immune systems by zooming into our micro security detail. We’d need an electron microscope to count our bodyguards!
A Quick Tour of The Immune System
The role of the immune system is to protect us from ‘bad stuff’ or pathogens: viruses, bacteria, or even our own cells gone rogue. Our immune system can recognize pathogens (also known as antigens) and trigger a defensive, response, such as the production of chemicals to destroy them. Antigens are recognized by our immune systems through antibodies. Think of them as molecular puzzle pieces with a shape that corresponds to that of an antigen. When that shape is filled, the antigen is able to activate an immune response1.
Innate and Adaptive Immunity
There are two kinds of immunity: innate and adaptive. As the name implies, we are born with innate immunity. It consists of a range of defenses: physical barriers like our skin, chemicals in our blood and also certain cells in the immune system. These processes are quick to activate but lack specificity; inflammation is one such process, where chemicals released by injured cells trigger a string of responses that causes redness, pain, and even fever.
Adaptive immunity is built up over time by learning. Our immune system can produce specific antibodies that serve as a form of memory. When the innate immune system encounters pathogens for the first time, it builds a library of antibodies, so that subsequent infection by the same pathogen is quickly suppressed. This is the reason why many illnesses (like measles) only occur once in a person’s life2.
Zooming Into Our Micro-Casino
Let’s put our security detail to good use by deploying them at a casino. As our immune system consists of many cells that have specific tasks to fulfill, so too does a casino’s security department. When a person is suspected of cheating or illegal entry, bouncers are the first on the scene, quickly apprehending the suspect. In the body, our ‘bouncers’ are cells from the innate immune system that jump on anything suspicious and destroy them.
In a casino, these suspects may be innocent patrons wrongly identified but thrown out anyway. Similarly, our innate immune system can trigger severe responses to otherwise harmless foreign particles (think allergies to dust or peanuts). Sometimes, the bouncers might be unsure if a suspect is actually cheating. They may choose to call in the higher-ups who are better equipped to decide.
Our Security Detail: Dendritic, B and T Cells
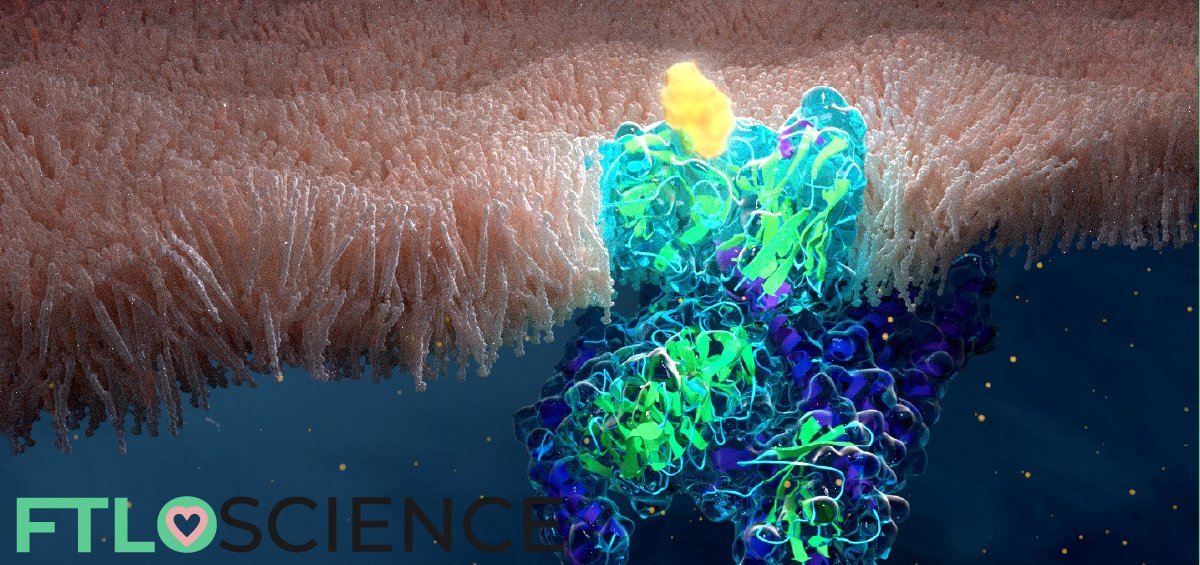
In the body, the cellular equivalent of these bouncers is our dendritic cells, serving as a link between the innate and adaptive immune systems. They engulf and transport the suspected antigen to specialized cells known as lymphocytes—B cells and T cells—that can differentiate and deal with the threat appropriately.
Dendritic cells do this by expressing the antigen (or part of it) on their membranes, allowing lymphocytes to correctly identify the culprits. In general, the difference between B and T cells is that B cells attack and inactivate an antigen directly, whereas T cells target host cells that have already been infected.
Dendritic cells, B cells and T cells work together to form the adaptive immune system. An important subgroup is the T helper cells, which are responsible for immunological ‘memory’. They are kept in the body for an extended period of time so that a returning antigen can be identified and destroyed quickly. Thus, cheaters are marked with a life-long house ban3,4.
But Does The House Always Win?
While we have many layers of security, due to the complexity of the system a small slip-up can have a massive impact on our body. Pathogens constantly develop ingenious ways to ‘trick’ our immune systems so that they can slip past undetected or delay our immune responses long enough to wreak havoc.
Bypassing Security Systems
Herpesviridae are a class of viruses that tend to infect a host for life, hiding out in the cells of the nervous system. By doing this, the immune system is unable to rid the body of the virus and proliferation can be re-activated in the future by stress or hormonal fluctuations5. These are known as latent infections and viruses from this family include the Epstein-Barr virus and the herpes simplex virus.
Our immune cells sometimes get too eager to take down threats and falsely recognize their fellow tissue cells as antigens. This results in autoimmune diseases, the root cause of which has not been identified yet. Thought to be connected to both genetic and external factors, interactions with antigens cannot be ruled out9,10.
One family of viruses that have gained notoriety for their ability to upset the balance of the immune system is the human immunodeficiency virus (HIV). An estimated 36.9 million people around the world are infected, with the resulting acquired immune deficiency syndrome (AIDS) claiming around one million lives per year6.
HIV Attacks the Immune System Itself
HIV attacks and enters specific cells that are key parts of the immune system itself such as T helper cells and dendritic cells. The virus inserts its own genome into the cell protein machinery by reverse-transcription and releases the copies, killing the host cell in the process7.
Naturally, this leads to a drop in immune cells, compromising immunity. If left untreated, it typically results in full-blown AIDS after 8-10 years. The immune system, therefore, doesn’t work the way it should and cannot protect the body against antigens; even the common cold can be a deadly threat 8.
An extremely quick replication cycle and a high chance of genome recombination mean there is a high rate of mutation of HIV’s protein structure. This makes it extremely difficult to develop an effective treatment for it, let alone a vaccine.
What Doesn’t Kill You Makes You Stronger?
The best way to strengthen our immune system is to present it with as many antigens as possible. After all, adaptive immunity has evolved for just this purpose. Exposure to bacteria, viruses and foreign particles allows the adaptive immune system to build up its ‘memory’, granting life-long immunity against these antigens. Studies have found that early age exposure to antigens lowers the chances of individuals developing allergies later in life11.
However, when an antigen is encountered, the process of developing adaptive immunity might take days or even weeks! Tuberculosis is one such example of a disease with a delayed immune response of up to 6 weeks12. This period of time allows for nasty symptoms to develop, damaging the body and sometimes overwhelming our immune system, leading to permanent damage or even death.
Supplementing Our Immune System with Vaccines
This is where vaccines come into play. Vaccination works by priming the body for high-risk antigens by producing helper T cells that can identify the virus. When we are infected by the real thing, we have a quicker immune response due to the presence of the corresponding antibodies.
Vaccines usually take the form of a small amount of a dead or inactivated antigen that is presented to our lymphocytes so that they induce ‘memory’ the same way an actual antigen might. The COVID-19 pandemic saw researchers use a variety of new techniques to develop a vaccine against the coronavirus.

Controversy Surrounding Vaccination
Vaccines have always been a hot topic in society, as well as the cause of controversy in the news and on social media. Despite the high-profile and mostly unfounded claims of the correlation between vaccines and autism (among other side effects), there is overwhelming evidence that vaccines have helped to eradicate certain diseases like smallpox and measles.
An outstanding example of the efficacy of vaccines can be seen in the smallpox virus. Smallpox went from infecting 50 million people every year to 0 in the span of 50 years (1948-1996), effectively eradicating the disease12,13. Without the discovery of vaccines, diseases like smallpox would have no doubt claimed the lives of millions more.
Vaccines represent advancements in medicine that are nothing short of medical miracles, so make sure you’re vaccinated! It’s the least you could do to help out your immune system that’s already fighting millions of pathogens on a daily basis.
Reference
- IQWiG (Institute for Quality and Efficiency in Health Care) (2016). How does the immune system work?
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology (2001). The Immune System in Health and Disease. 5th edition. New York: Garland Science. The course of the adaptive response to infection.
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology (2001). The Immune System in Health and Disease. 5th edition. New York: Garland Science. The components of the immune system.
- Janeway CA Jr, Travers P, Walport M, et al. Immunobiology (2001). The Immune System in Health and Disease. 5th edition. New York: Garland Science. Immunological memory.
- Arvin A, Campadelli-Fiume G, Mocarski E, et al., editors (2007). Human Herpesviruses: Biology, Therapy, and Immunoprophylaxis. Cambridge: Cambridge University Press. Chapter 26.
- UNAIDS (2018): Global HIV & AIDS statistics ? 2018 fact sheet.
- Cummins, N. W., & Badley, A. D. (2014). Making sense of how HIV kills infected CD4 T cells: implications for HIV cure. Molecular and Cellular Therapies, 2, 20.
- IARC Working Group on the Evaluation of Carcinogenic Risk to Humans (1996). Human Immunodeficiency Viruses and Human T-Cell Lymphotropic Viruses. Lyon (FR). International Agency for Research on Cancer. (IARC Monographs on the Evaluation of Carcinogenic Risks to Humans, No. 67.) 1, Exposure Data.
- Arango MT, Shoenfeld Y, Cervera R, et al. Infection and autoimmune diseases. In: Anaya JM, Shoenfeld Y, Rojas-Villarraga A, et al., editors (2013). Autoimmunity: From Bench to Bedside [Internet]. Bogota (Colombia): El Rosario University Press. Chapter 19.
- National Institute of Environmental Health Sciences (2018). Autoimmune Diseases.
- Graham A W Rook, Laura Rosa Brunet (2014). Give us this day our Daily Germs. Royal Free and University College Medical School, London, UK.
- Urdahl, K. (2015) Understanding the Immune Response to M. tuberculosis. Nature Education 8(3):6
- Unicef (1996). Vaccines bring 7 diseases under control.
- World Health Organization: Bugs, drugs and smoke (2011). stories from public health. Chapter 1
About the Author

Katharina was a science writer at FTLOScience from July 2018 to October 2019.