The smallpox virus terrorized humankind for thousands of years. Even if victims survived the infection, smallpox often led to permanent blindness and disfigurement. This plague upon humanity finally ended in 1980 after a worldwide vaccination drive, completely wiping out the disease. More than 40 years later, it remains the only human disease ever eradicated. However, we can still learn a lot from this success and apply them to current issues such as monkeypox, coronavirus and vaccine development.
Origins of the Smallpox Virus
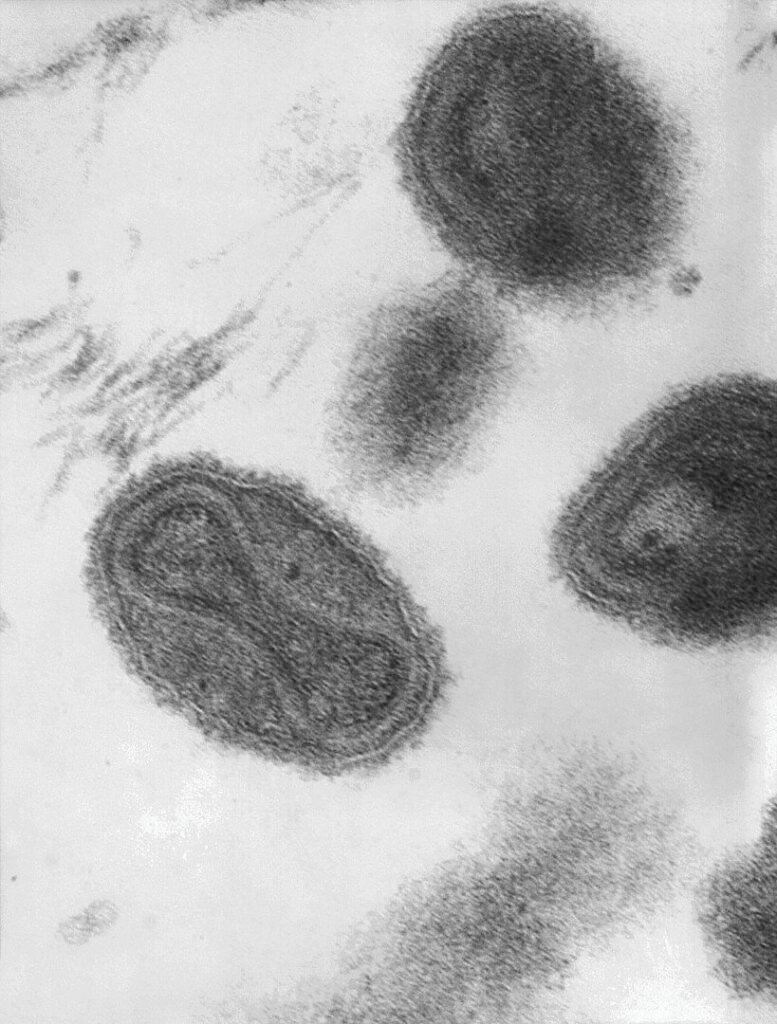
Thought to have originated from rodents thousands of years ago, the smallpox virus is a brick-shaped virus containing a single DNA strand. It belongs to the family of poxviruses, which includes cowpox, horsepox and monkeypox (though not chickenpox). Like other viruses, it takes over the host cells’ replication machinery to make copies of itself.
From 1880 to 1980, the smallpox virus (Variola major and Variola minor) is estimated to have killed up to 500 million people, much more than all the deaths caused by all wars in the same period. As a virus, smallpox is highly contagious among humans. After infection, the virus attacks skin cells, leading to the characteristic red lesions that cover the patient’s body. Smallpox infection has no cure, with an overall fatality rate of 30%, while certain hemorrhagic forms of the virus are almost always fatal.
Long Road to Smallpox Eradication
Early Inoculation Techniques
There have been reports of inoculation from as early as the 16th century in Ming dynasty China. Doctors would introduce the less severe strain of the virus (Variola minor) to patients, in the hopes of priming their immune system in the case of infection by the more severe Variola major. This would mark the beginnings of the smallpox vaccine—and the birth of vaccination as a therapeutic technique.
Infecting patients with Variola minor was a risky process, however, as severe side effects could still result from the smallpox virus. In 1796, British doctor Edward Jenner realized that his patients who had earlier in their lives contracted cowpox (from the same family as the smallpox virus) would be protected from smallpox infection. He proceeded to purposefully infect people with the fluid from the lesions of patients suffering from cowpox, in what is often portrayed as the first form of successful vaccination. The word vaccine is derived from Vacca, which is Latin for cow!
Three Generations of Smallpox Vaccines
Jenner’s technique worked, but there was much controversy about using humans suffering from cowpox as the source of inoculation material. In 1939, it was discovered that another species of poxvirus—vaccinia—was more closely related to smallpox than cowpox, offering better protection. This virus was cultured on the skin of sheep and cows, being extracted as and when they were needed. These skin extracts are considered first-generation smallpox vaccines.
The problem with using animals was that their skin often carried other pathogens. It wasn’t possible to disinfect the solution beforehand because this would also inactivate the virus that would provide immunity. This led to the use of bacterial cell cultures to generate the virus, in what would be known as second-generation vaccines. Second-generation vaccines could be produced in a sterile environment since the bacteria could be inactivated with specific antibiotics. However, because the live virus was administered, there was still the issue of side effects and possible contagion. This prompted the development of third-generation vaccines.
Third-generation smallpox vaccines are those that use genetically modified forms of the vaccinia virus. Several vaccines of this sort were developed and refined, reducing the amount and severity of side effects while ensuring they offered sufficient protection against the smallpox virus. One such vaccine, developed by English microbiologist Leslie Collier in the late 1950s,prompted the World Health Organization to embark on a worldwide vaccination drive.

Worldwide Vaccination Campaign
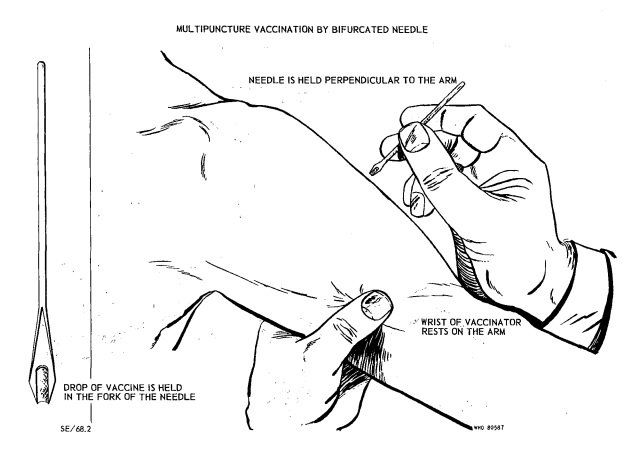
Leslie Collier’s smallpox vaccine was unique; it could be dried and stored for months at temperatures up to 37 °C, allowing it to be transported worldwide. Combined with the development of a superior method of vaccination—the bifurcated needle—it was possible to vaccinate large populations quickly and efficiently.
The worldwide vaccination campaign began in 1967, requiring hundreds of millions of vaccine doses. At the time, there were still tens of millions of smallpox cases yearly. However, the vaccine and its rollout were so effective that by 1971, the virus had been eradicated from the Americas. South-east Asia (1972) and the rest of Asia (1975) followed suit. Smallpox would be eliminated in Africa in 1977, and after several years without an outbreak, the virus was officially declared eradicated in 1980.
Those involved in the vaccination campaign were awarded the ‘Order of the Bifurcated Needle’, a lapel badge made from a bifurcated needle bent to form the shape of an ‘O’, signifying the eradication of the once deadly smallpox virus.
Lesson We Can Learn from the Smallpox Virus
Similarities to Monkeypox
The 2022 monkeypox outbreak raised fears over a possible smallpox-level transmission event, leading to the World Health Organization declaring it a public health emergency of international concern. As usual, news and social media outlets were quick to stretch the truth, painting a much deadlier image of the virus than experts predicted.
Smallpox and monkeypox belong to the same family of poxviruses, which means smallpox vaccines would theoretically work well against monkeypox. However, since smallpox was eradicated in 1980, we no longer practice systematic vaccination. This has led to a ‘gap’ in our immunity, making us susceptible to monkeypox infection.
So, do we need to start another vaccination drive? The sudden spike in monkeypox cases might suggest so. However, monkeypox isn’t as contagious as smallpox. It is mainly spread through prolonged skin contact, usually of a sexual nature. More importantly, monkeypox isn’t nearly as deadly as smallpox, with a fatality rate of 3–6%. Because of this, only select healthcare personnel require vaccination, although this might change in the future.
Applications to the Coronavirus
There is still much controversy surrounding vaccination, especially with the mass vaccination drives against the SARS-CoV-2 virus (coronavirus) today. Anti-vaxxers spread misinformation about autism and other side effects of vaccination, and we are not helped by the poor efficacy of the current crop of coronavirus vaccines. People use the fact that they can still get infected even after vaccination as evidence that vaccines don’t work. Or exaggerate the side effects of receiving the vaccines.
Vaccine development is a slow process, taking an average of 15 years for a single vaccine to go from discovery to market. Vaccines are subject to more stringent requirements than regular drugs because they are administered on a larger scale to the uninfected population; the tolerance for error is much lower. But we can’t expect a perfect iteration immediately.
Remember that it took hundreds of years to develop the third-generation smallpox vaccines that provided the best protection with minimal side effects. Though the drug development landscape has changed since then, it will likely take much more research to uncover an ideal vaccine that confers complete immunity against the coronavirus. However, when we get there, the coronavirus’ days will surely be numbered.
Dangers of Biological Weapons
When smallpox was confirmed eradicated in 1980, all virus samples were promptly ordered to be destroyed. However, samples are maintained by the U.S. Center for Disease Control (CDC) and the Russian State Research Center (VECTOR) for ‘research’ purposes. They serve no benefit against further smallpox outbreaks since vaccine research and manufacturing today are not dependent on live samples of the virus. However, neither group is willing to dispose of their samples while the other still possesses them.
This is controversial, as it raises the concern of using these stockpiles as biological weapons. Though bioweapons have been outlawed—twice, in 1925 and then again in 1972—this has not stopped countries from researching and manufacturing them. During the cold war, the Soviet Union amassed large stockpiles of live smallpox virus, planning to use them in combination with intercontinental ballistic missiles.
Even more worrying is the possibility that vaccine-resistant strains of smallpox could be genetically engineered, which would make hundreds of years of medical research redundant if released into the world. Because of this, the World Health Organization (WHO) has banned all research related to genetic engineering of the smallpox virus.
The Power of Vaccination
The history of smallpox is a testament to the effectiveness of vaccination as a medical intervention. Smallpox was the first human virus to be wiped off the face of the Earth and, at the time of writing, remains the only human virus officially declared eradicated. The eradication of smallpox is one of modern medicine’s greatest success stories, up there with the mass production of Penicillin.
Though it took us thousands of years to find an inoculation, and a further hundred or so years to perfect it, the discovery and development of vaccination techniques have given us a powerful tool in the fight for improving human health. It is the hope that the lessons learned from the smallpox virus can help to similarly wipe deadly diseases—of both present and future—off the face of the Earth.
About the Author

Sean is a consultant for clients in the pharmaceutical industry and is an associate lecturer at La Trobe University, where unfortunate undergrads are subject to his ramblings on chemistry and pharmacology.




